- sales@willychemicals.com
- 1-240-401-4525
- Mon - Fri 09:00 - 18:00
Treatment restores blood vessel growth, muscle vitality, boosts exercise endurance in aging animals
We are as old as our arteries, the adage goes, so could reversing the aging of
blood vessels hold the key to restoring youthful vitality?
The answer appears to be yes, at least in mice, according to a new study led by
investigators at Harvard Medical School.
The research, published March 22 in Cell identifies the key cellular
mechanisms behind vascular aging and its effects on muscle health and has
successfully reversed the process in animals.
The findings pinpoint a glitch in the normal crosstalk that occurs between muscles and blood vessels and keeps both tissues healthy.
Using the synthetic precursors of two molecules naturally present in the body,
the scientists also managed to reverse blood vessel demise and muscle atrophy in
aging mice, boosting their exercise endurance in the process.
The achievement, the team said, paves the way to identifying related therapies
for humans.
“We’ve discovered a way to reverse vascular aging by boosting the presence of
naturally occurring molecules in the body that augment the physiological
response to exercise,” said study senior investigator David Sinclair,
professor in the Department of Genetics at Harvard Medical
School and co-director of the Paul F. Glenn Center for the Biology of Aging at
Harvard Medical School.
“The approach stimulates blood vessel growth and boosts stamina and endurance in mice and sets the stage for therapies in humans to address the spectrum of diseases that arise from vascular aging,” added Sinclair, who is also a professor at the University of New South Wales School of Medical Sciences in Sydney, Australia.
The researchers caution that many promising treatments in mice don’t have the same effect in humans due to critical differences in biology. However, the results of the experiments were dramatic enough to prompt the research team to pursue experiments in humans. Clinical trials for safety are already under way, Sinclair said.
As old as our blood vessels
Sinclair and team set out to unravel the mechanisms behind one of biology’s
inevitabilities: aging.
As we grow old, we become weak and frail. A constellation of physiological
changes—some subtle, some dramatic—precipitate this inevitable decline. What
exactly happens inside our cells to cause the biological shifts that lead to
aging? It’s a question that has vexed Sinclair and team for years.
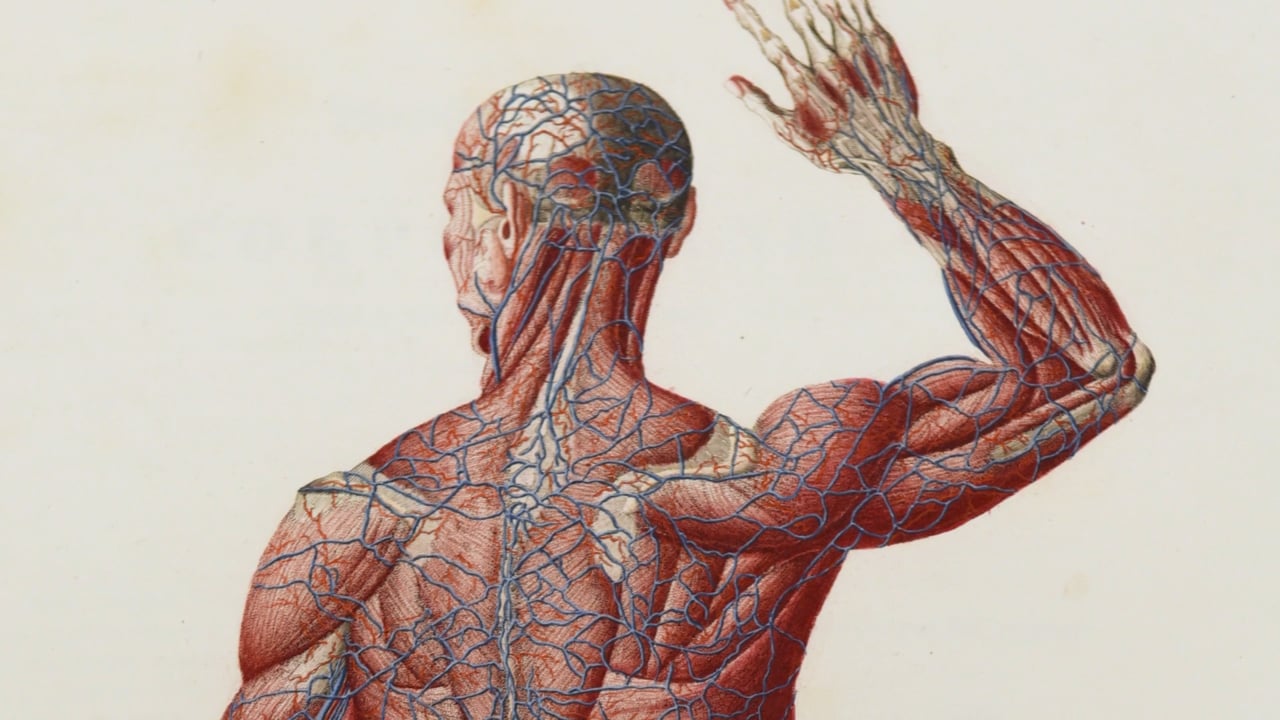
As we age, our tiniest blood vessels wither and die, causing reduced blood flow
and compromised oxygenation of organs and tissues. Vascular aging is responsible
for a constellation of disorders, such as cardiac and neurologic conditions,
muscle loss, impaired wound healing and overall frailty, among others.
Scientists have known that loss of blood flow to organs and tissues leads to the
build-up of toxins and low oxygen levels. The so-called endothelial cells, which
line blood vessels, are essential for the health and growth of blood vessels
that supply oxygen-rich and nutrient-loaded blood to organs and tissues. But as
these endothelial cells age, blood vessels atrophy, new blood vessels fail to
form and blood flow to most parts of the body gradually diminishes. This dynamic
is particularly striking in muscles, which are heavily vascularized and rely on
robust blood supply to function.
Muscles begin to shrivel and grow weaker with age, a condition known as
sarcopenia. The process can be slowed down with regular exercise, but gradually
even exercise becomes less effective at holding off this weakening.
Sinclair and team wondered: What precisely curtails the blood flow and
precipitates this unavoidable decline? Why does even exercise lose its
protective power to sustain muscle vitality? Is this process reversible?
In a series of experiments, the team found that reduced blood flow develops as
endothelial cells start to lose a critical protein known as sirtuin1, or SIRT1.
Previous studies have shown that SIRT1 delays aging and extends life in yeast
and mice.
SIRT1 loss is, in turn, precipitated by the loss of NAD+, a key regulator of
protein interactions and DNA repair that was identified more than a century ago.
Previous research by Sinclair and others has shown that NAD+, which also
declines with age, boosts the activity of SIRT1.
A stimulating conversation
The study reveals that NAD+ and SIRT1 provide a critical interface that enables the conversation between endothelial cells in the walls of blood vessels and muscle cells.
Specifically, the experiments reveal that in young mouse muscle, SIRT1 signaling
is activated and generates new capillaries, the tiniest blood vessels in the
body that supply oxygen and nutrients to tissues and organs. However, as
NAD+/SIRT1 activity diminishes over time, the study found, so does the blood
flow, leaving muscle tissue nutrient-deprived and oxygen-starved.
Indeed, when researchers deleted SIRT1 in the endothelial cells of young mice,
they observed markedly diminished capillary density and decreased number of
capillaries, compared with mice that had intact SIRT1. Mice whose endothelial
cells lacked SIRT1 had poor exercise tolerance, managing to run only half the
distance covered by their SIRT1-intact peers.
To determine SIRT1’s role in exercise-induced blood vessel growth, the
researchers observed how SIRT1-deficient mice responded to exercise. After a
month-long training regimen, the hind-leg muscles of SIRT1-deficient mice showed
markedly diminished ability to form new blood vessels in response to exercise
compared with same-age mice that had intact SIRT1 in their endothelial
cells.
Exercise-induced blood vessel formation is known to occur in response to
growth-stimulating proteins released by muscles under strain. SIRT1, however,
appears to be the key messenger relaying growth-factor signaling from muscles to
blood vessels, the study found.
Experiments showed that endothelial cells lacking SIRT1 were desensitized to the
growth-stimulating proteins released by exercised muscles.
“It’s as if these cells had grown deaf to the signals that muscles sent their
way,” Sinclair said.
The observation, he added, explains why age-related loss of SIRT1 leads to
muscle atrophy and blood vessel demise.
Since the experiments revealed the critical role of SIRT1 in exercise-induced
blood vessel formation, the researchers wondered whether boosting SIRT1 levels
would stimulate blood vessel growth and stave off muscle wasting.
Exercise in a pill?
The scientists set their sights on NAD+, a molecule conserved across many life forms, known to decline with age and previously shown to stimulate SIRT1 activity.
“We reasoned that declining NAD+ levels reduce SIRT1 activity and thus interfere with aging mice’s ability to grow new blood vessels,” said study first author Abhirup Das, who conducted the work as a post-doctoral fellow in Sinclair’s lab, currently a visiting scholar in genetics at Harvard Medical School and a post-doctoral research fellow at the University of South New Wales School of Medical Sciences.
To test this premise, scientists used a chemical compound called NMN, a
NAD+ precursor, previously
shown to play a role in repairing cellular DNA and maintaining cell
vitality.
In lab dish experiments, endothelial cells from humans and mice treated with NMN
showed enhanced growth capacity and reduced cell death.
Next, the team gave NMN over two months to a group of mice that were 20 months
old—the rough equivalent of 70 in human years. NMN treatment restored the number
of blood capillaries and capillary density to those seen in younger mice. Blood
flow to the muscles also increased and was significantly higher than blood
supply to the muscles seen in same-age mice that didn’t receive NMN.
The most striking effect, however, emerged in the aging mice’s ability to
exercise. These animals showed between 56 and 80 percent greater exercise
capacity, compared with untreated mice the study showed. The NMN-treated animals
managed to run 430 meters, or about 1,400 feet, on average, compared with 240
meters, or 780 feet, on average, for their untreated peers.
To see whether the effects of NMN could be further augmented, the researchers
added a second compound to the treatment regimen. The compound, sodium
hydrosulfide (NaHS), is a precursor to hydrogen sulfide, which also boosts the
activity of SIRT1.
A group of 32-month-old mice—the rough equivalent to 90 in human years—receiving the combo treatment for four weeks were able to run, on average, twice as long as untreated mice. In comparison, mice treated with NMN alone ran 1.6 times farther, on average, than untreated animals.
“These are really old mice so our finding that the combo treatment doubles their
running capacity is nothing short of intriguing,” said study co-author James
Mitchell,
associate professor of genetics and complex diseases at the Harvard T. H. Chan
School of Public Health. Research led by Mitchell and published in the
same issue of Cell also found sodium hydrosulfide to augment
blood vessel formation in the muscles of mice.
Interestingly, the NMN treatment did not improve blood vessel density and
exercise capacity in young sedentary mice. However, it did boost blood vessel
formation and exercise capacity in young mice that had been exercising regularly
for a month.
“This observation underscores the notion that age plays a critical role in the
crosstalk between blood vessels and muscles and points to a loss of
NAD+ and SIRT1 as the reason behind loss of exercise
effectiveness after middle age,” Das said.
The researchers say their findings may pave the way to therapeutic advances that hold promise for the millions of older people for whom regular physical activity is not an option.
“Even if you’re an athlete, you eventually decline,” Sinclair said. “But there is another category of people—what about those who are in a wheelchair or those with otherwise reduced mobility?”
The team’s ultimate goal is to replicate the findings and, eventually, move
toward developing small-molecule, NMN-based drugs that mimic the effects of
exercise—enhanced blood flow and oxygenation of muscles and other tissues. Such
therapies may even help with new vessel growth of organs that suffer
tissue-damaging loss of blood supply and oxygen, a common scenario in heart
attacks and ischemic strokes, the team said.
Neo-vascularization—the formation of new blood vessels—should be treated with
caution, the researchers say, because increased blood supply could inadvertently
fuel tumor growth.
“The last thing you want to do is provide extra blood and nourishment to a tumor if you already have one,” said study co-author Lindsay Wu, at the University of New South Wales School of Medical Sciences.
Sinclair and Wu point out that experiments done as part of the current study provide no evidence that treatment with NMN stimulated tumor development in animals treated with the compound.
Co-investigators included George Huang, Michael Bonkowski, Alban Longchamp,
Catherine Li, Michael Schultz, Lynn-Jee Kim, Brenna Osborne, Sanket Joshi,
Yuancheng Lu, Jose Humberto, Trevine-Villareal, Myung-Jin Kang, Tzong-tyng Hung,
Brendan Lee, Eric Williams, Masaki Igarashi, James Mitchell, Nigel Turner, Zolt
Arany and Leonard Guarente.
The work was supported by the Glenn Foundation for Medical Research (grants RO1
AG028730 and RO1 DK100263), and by the National Institutes of Health/National
Heart, Lung and Blood Institute (grant RO1 HL094499).
Relevant disclosures:
Sinclair and Wu are consultants and inventors on patents licensed to Metro International Biotech, JumpStart Fertility, Vium, Life Biosciences and Liberty Biosecurity. Sinclair is consultant to EdenRoc Sciences, Arc Bio, Segterra, Animal Biosciences, Senolytic Therapeutics, Spotlight Biosciences and Continuum Biosciences. Wu is consultant to Intravital and JumpStart Fertility. Bonkowski is a consultant to Metro International Biotech. Sinclair sits on the fiduciary board and has an equity interest in EdenRoc Sciences, Arc Bio, Segterra, Metro International Biotech, Liberty Biosecurity, Animal Biosciences, Life Biosciences, Senolytic Therapeutics, Spotlight Biosciences and Continuum Biosciences. He is a cofounder of EdenRoc Sciences, Arc Bio, Metro International Biotech, Liberty Biosecurity, Life Biosciences, and Spotlight Biosciences. Guarente is advisor to Segterra, Sebelius and Elysium Health. A provisional patent application has been submitted with Das, Wu and Sinclair as inventors.